Insurance Eligibility and Benefits Verification
Eligibility Verification and Prior Authorization
Eligibility and insurance verification are vital to ensuring accurate and timely receipt of information regarding insurance coverage. Without proper checks and balances in place, a healthcare organization could be leaving money on the table. Failure to confirm eligibility and achieve prior authorization can lead to delayed payments and denials, resulting in decreased collections and revenues.
Eligibility verification processes help healthcare providers submit clean claims. It avoids claim resubmission, reduces demographic or eligibility-related rejections and denials, increases upfront collections; leading to improved patient satisfaction and improving medical billing.
Leverage Maxx Healthcare’s Eligibility Verification and Prior Authorization services to optimize your revenue cycle and improve collections.
ELIGIBILITY AND BENEFITS VERIFICATION SERVICES
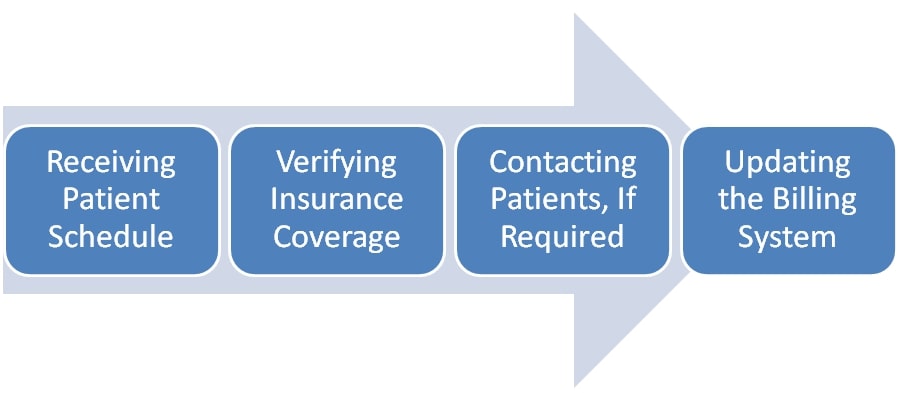
Workflows received through the patient scheduling system, EDI, Fax, emails, and FTP files
Accurate verification of primary and secondary coverage details, including member ID, group ID, coverage period, co-pay, deductible, and co-insurance and benefits information
Efficient connection with the payer using the best possible channel (phone or web)
Prompt identification and resolution of missing or invalid data
Upgrade eligibility verification processes with our proprietary RPA tools
PRIOR AUTHORIZATION
Rapid determination of prior authorization requirements
Prepare and submit paperwork to the payer
Consistent follow-ups on submitted prior-authorization requests
Immediate notification of any issues with the authorization request
MAXX HEALTHCARE’S VALUE PROPOSITION FOR ELIGIBILITY VERIFICATION SERVICES
Optimized cash flow
Reduced patient-related denials
Avoided rejection of claims by payers due to inaccurate or incomplete information
Identification of the patient’s responsibility upfront
Improved patient satisfaction
Contact us to learn how your organization can leverage Maxx Healthcare’s Prior Authorization Services.
